What is diabetes?
Diabetes mellitus, more commonly known simply as diabetes, is a health condition where there is too much sugar in your blood.
People with diabetes have difficulty changing glucose (a type of sugar) into energy. This leads to high levels of sugar in your blood (hyperglycaemia).
Your blood glucose levels are normally controlled by a hormone called insulin. Diabetes happens when your pancreas can’t produce enough insulin or when your body can’t use the insulin because it’s resistant to it.
There are several types of diabetes:
type 1 diabetes
type 2 diabetes
gestational diabetes, which happens when a woman has high blood glucose levels during pregnancy
pre-diabetes, where your blood glucose levels are higher than normal, but not high enough for a diagnosis of diabetes
What are the symptoms of diabetes?
Common symptoms of diabetes are:
being very thirsty or hungry
passing more urine (wee) than usual
feeling tired
unexplained weight loss (for type 1 diabetes), or gradual weight gain (for type 2 diabetes)
having cuts that heal slowly
itchy skin or skin infections
blurred vision
Type 1 diabetes is usually spotted quickly as symptoms can appear suddenly.
Many people with type 2 diabetes:
don’t have any symptoms at all
have signs that go unnoticed for a long time
CHECK YOUR SYMPTOMS — Use the Symptom Checker and find out if you need to seek medical help.
What causes diabetes?
There are different causes of diabetes according to the type.
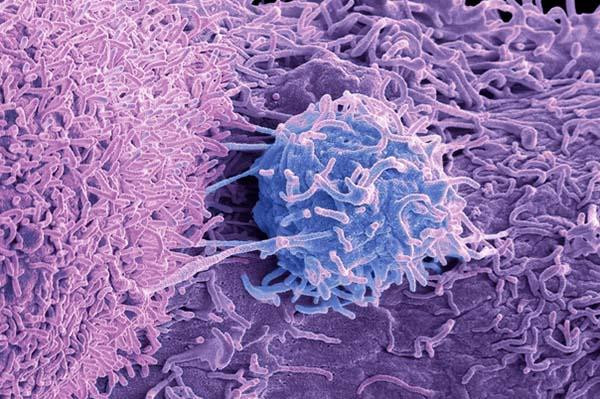
Type 1 diabetes
Type 1 diabetes is an auto-immune condition: your body’s immune system attacks the cells in your pancreas that produce insulin.
The exact cause of this reaction is still unknown. Diet and lifestyle are not factors that determine who gets type 1 diabetes. Research shows that both your genetics and the environment may play a part in the development of type 1 diabetes.
Type 2 diabetes
Type 2 diabetes happens slowly over years as your body’s insulin becomes less effective at managing your blood glucose levels.
As a result, your pancreas produces more and more insulin. Eventually your insulin producing cells wear out and become ineffective. Type 2 diabetes is a mix of low insulin and ineffective insulin.
The risk of getting type 2 diabetes increases with certain factors:
a family history of diabetes
low levels of physical activity
poor diet
being obese or overweight, especially around your waist
having high blood pressure
NEED TO LOSE WEIGHT? — Use the BMI Calculator to find out if your weight and waist size are in a healthy range.
Gestational diabetes
During pregnancy, hormones that give nutrition to your growing baby reduce the effectiveness of your own insulin.
If your pancreas is unable to produce enough insulin, your blood glucose levels rise and you get gestational diabetes.
When should I see my doctor?
See your doctor if you are experiencing symptoms of diabetes or have concerns about your risk of diabetes.
Early diagnosis and treatment can help to reduce your risk of serious complications.
How is diabetes diagnosed?
If your doctor suspects that you have diabetes, they will order blood tests. These will check your glucose levels.
This may include the following tests.
Blood glucose test — this may be done after fasting (not eating for a few hours) or without any special preparation (random or non-fasting blood glucose test).
Oral glucose tolerance test (OGTT) — this involves drinking a sugary drink, then testing your glucose levels 1 to 2 hours later.
HbA1c test — this test doesn’t need you to fast as it doesn’t test your glucose levels directly. It shows how much sugar there has been in your blood over the past few months.
If you’re pregnant, your doctor will screen for gestational diabetes as part of your standard antenatal testing.
How is diabetes treated?
Although there is no cure for diabetes it can be managed with lifestyle changes and medicines.
Type 1 diabetes
If you have type 1 diabetes, you will need to have insulin replacement. This may be through injections or an insulin pump. This helps control your body’s blood glucose levels.
There’s nothing you can do to prevent type 1 diabetes. However, your lifestyle choices after your diagnosis can lower your risk of getting complications.
Type 2 diabetes
Type 2 diabetes can sometimes be controlled by lifestyle changes, such as eating a healthy diet and being physically active.
Eventually, you may need to take medicines to control your blood glucose levels. Your doctor may prescribe tablets or injectable medicines (insulin or others). These will help to keep your blood glucose in the target range.
Gestational diabetes
Gestational diabetes can often be managed by keeping blood glucose levels within a healthy range for pregnancy.
This involves a healthy eating plan and regular physical activity.
You may need medicine if you don’t get good glucose control with lifestyle changes alone.
Blood glucose monitoring
Regular blood glucose monitoring is crucial to diabetes management. This helps you to understand the relationship between your blood glucose, food, exercise and insulin in your body.
It also helps you keep track of potential treatment side effects, such as hypoglycaemia (a sudden drop in blood sugar).